Low occurrence of colectomy with long-term (up to 4 years) golimumab treatment in patients with moderate-to-severe active Ulcerative Colitis: Data from the PURSUIT maintenance and long-term extension studiesYear: 2022
Source: ECCO'22 Virtual
Authors: Cindy L.J. Weinstein
Created: Tuesday, 24 May 2022, 8:13 PM
BackgroundIn a previous real-world study of long-term (up to 4 years) treatment with golimumab (GLM) in ulcerative colitis (UC), patients reported a low overall colectomy incidence (5.8%).1 This analysis evaluates the incidence of colectomy among patients with moderate-to-severe active UC in the PURSUIT-maintenance (-M)2 and long-term extension (-LTE)3 studies.
MethodsEligible PURSUIT-M trial participants completed a 6-week GLM induction trial without requiring colectomy.4,5 Responders to GLM induction were randomised 1:1:1 to GLM 50 mg, 100 mg, or placebo (PBO) maintenance for up to 1 year, administered every 4 weeks (q4w). Nonresponders to GLM or PBO induction received GLM 100 mg; responders to PBO induction received PBO (each administered q4w for up to 1 year). Participants experiencing loss of clinical response during maintenance were eligible for one treatment intensification (switch from PBO to GLM 100 mg, or GLM dose increase). Participants who completed PURSUIT-M were eligible to continue their treatment in the 3-year PURSUIT-LTE study. Colectomy (total or partial) was a prespecified outcome in PURSUIT-M; serious adverse event narratives and safety summaries were also examined for reports of colectomy (total or partial). For PURSUIT-LTE, serious adverse event narratives and safety summaries were examined for reports of colectomy (total or partial). The reasons for colectomy were not collected systematically in PURSUIT-M or -LTE. Descriptive information on colectomies was assessed and reported.
ResultsA total of 60 (4.9%) colectomies were reported among the 1228 patients who enrolled in the 1-year PURSUIT-M study, including 672 participants who continued into the 3-year LTE study. The table shows the distribution of colectomies by study phase, induction responder status, initial treatment assignment, and treatment prior to colectomy. The colectomy rate during the 3-year extension was lower than that observed during the maintenance phase of the study [1.3% (9/672) compared to 4.2% (51/1228)].

ConclusionConsistent with previously reported data, this retrospective evaluation of colectomy data from the PURSUIT-M and -LTE studies in patients with moderate-to-severe active UC demonstrated a low occurrence of colectomy with long-term (up to 4 years) GLM treatment. The limited number of colectomies observed in the LTE study occurred predominantly in patients with more severe disease at baseline (induction non-responders) who had been receiving GLM 100 mg.
References:
1. Iborra M, et al. SciRep. 2020;10:17774
2. Sandborn WJ, et al. Gastroenterol. 2014;146:96–109
3. Reinisch W, et al. J Crohn's Col. 2018;12:1053–1066
4. Sandborn WJ, et al. Gastroenterol. 2014;146:85–95
5. Rutgeerts P, et al. Aliment Pharmacol Ther. 2015;42:504–514
Luminal Crohn's disease e-CourseYear: 2020
Source: e-Course
Authors: João Sabino, Bram Verstockt, Kostas Katsanos, Pascal Juillerat, Pierre Ellul
Created: Friday, 28 February 2020, 11:33 AM by Dauren Ramankulov
Last Modified: Wednesday, 2 June 2021, 1:58 PM by ECCO Administrator
This course has been developed by physicians who had recently participated in the writing of the ECCO Crohn's disease consensus Guidelines. This course is intended for those who are interested in Inflammatory Bowel Disease(s) (IBD). One major aim of this e-learning activity is to increase competence and knowledge with regard to Luminal disease in order to improve patient outcomes.
Upon completion of this case you will:
- Know the evidence for induction of remission in mild-to-moderate Crohn’s disease;
- Know the evidence for maintaining remission in Crohn’s disease;
- Know the evidence on how to react upon disease flares, immediately after induction therapy or during maintenance therapy;
- Understand the benefits and risks of several medical therapies;
- Achieve familiarity how to use immunomodulatory agents in mono- or combination therapy;
- Achieve familiarity how to monitor Crohn’s disease patients who initiated medical therapy or who underwent surgery;
- Recognise indications for surgical management.
Maintenance of Remission e-CourseYear: 2015
Source: e-Course
Authors: Gerassimos J Mantzaris, Joana Torres, and Monica Cesarinni
Created: Thursday, 27 February 2020, 4:42 PM by Dauren Ramankulov
Last Modified: Monday, 17 August 2020, 10:27 AM by Dauren Ramankulov
This course is designed for gastroenterologists, surgeons, and other interdisciplinary medical experts interested in IBD. The intended result of this activity is increased competence, knowledge, performance and improved patient outcome.
Upon completion of this activity learners will:
- Be aware of current treatment options for Crohn's disease
- Be able to understand treatment options are based on disease severity and prognostic factors at disease presentation
- Be able to understand the therapeutic choices for maintaining remission of disease
- Know how to prevent and treat the main adverse events related to drug therapy
- Manage maintenance therapy in special situations
Maintenance phase propensity score adjusted effectiveness and persistence at week-52 in biologic-naïve Ulcerative Colitis patients treated with vedolizumab or anti-TNF (VEDO IBD-study)Year: 2022
Source: ECCO'22 Virtual
Authors: Bernd Bokemeyer
Created: Tuesday, 24 May 2022, 8:13 PM
BackgroundIn this real-world-evidence (RWE) study we aimed to analyse the persistence of biologic therapy in biologic-naïve ulcerative colitis (UC) patients and to compare 1-year effectiveness of vedolizumab (VDZ) and anti-TNF.
MethodsBetween 2017 and 2020, 1200 consecutively enrolled biologic-naïve and biologic- experienced patients with UC and Crohn´s disease (CD) were prospectively included in the VEDOIBD-Registry from 45 IBD-experienced centres across Germany. After exclusion of bio-experienced patients, CD and missing outcomes, the final sample consisted of 274 biologic-naïve UC-patients with 1-year follow-up data. Switchers of a drug were considered as treatment failure (modified intention-to-treat analysis; mITT) while switchers were excluded from per protocol analysis (PP). Clinical response modified (reduction of partial Mayo score (pMayo) from baseline to 1-year by >3 points or a reduction of at least 30% compared to baseline or reaching remission at 1-year) and (steroid-free) remission rates (pMayo ≤1 plus a bleeding subscore=0 (and no systemic use of steroids or budesonide at 1-year)) were predefined as outcomes. To reduce the effect of confounders, PS adjustment with inverse probability of treatment weighting (IPTW) was implemented. A weighted logistic regression was used, and the results were reported as odds ratio (OR) and 95% confidence interval (CI).
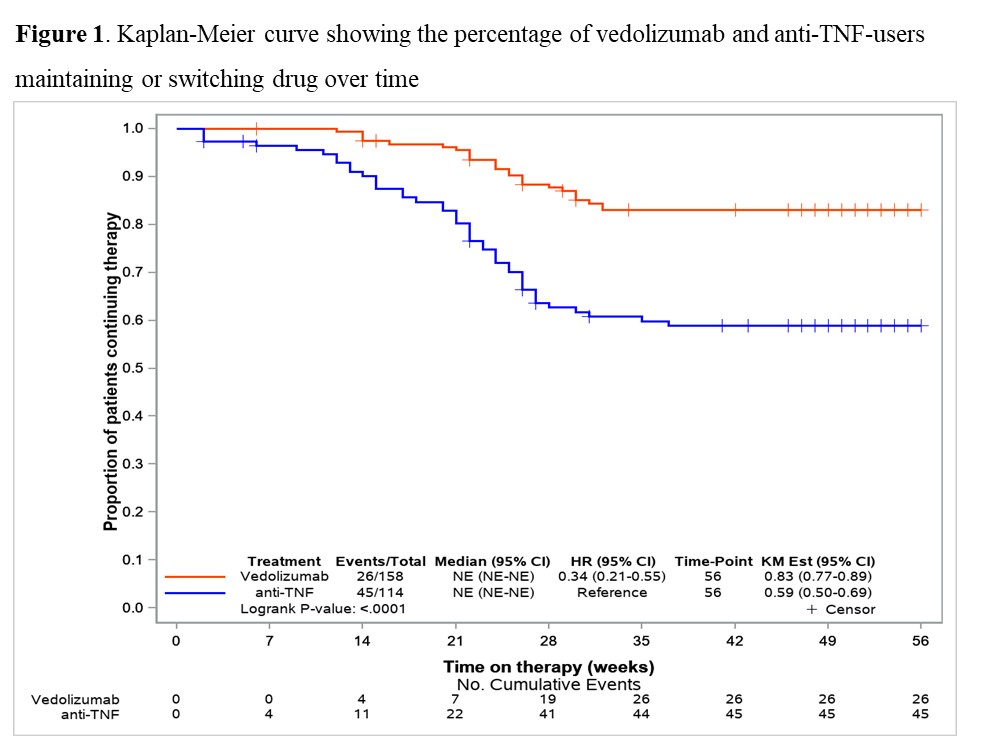
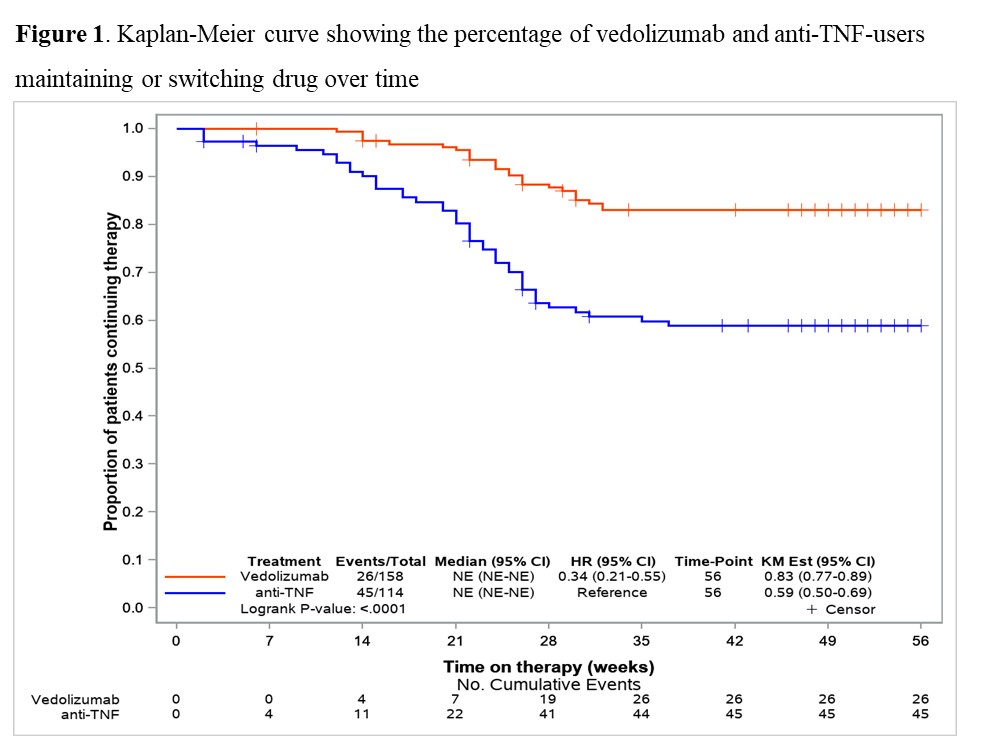
Results158 VDZ and 116 anti-TNF (ADA: 27.6%, IFX: 57.8%, GOL: 14.7%) biologic-naïve UC-patients were included in this prospective RWE comparing the effectiveness of VDZ vs anti-TNF. Until week 52 significantly more patients switched to another biologic-drug in the anti-TNF group than in the VDZ group (40.5% vs 16.5%; p<0.001) (Fig. 1). In mITT, clinical response at 1-year was significantly higher in VDZ than in anti-TNF treated patients (61.7% vs. 40.3%; OR 2.39 (95% CI 1.39-4.10)). VDZ also tended to be superior to anti-TNF for (steroid-free) remission (Tab. 1; p=0.058 (p=0.051)). In the PP-analysis, VDZ showed numerically higher 1-year effectiveness, but this did not reach statistical significance (Tab. 1). Analysing week-14 induction phase responders (Tab. 2), VDZ had numerically higher effectiveness rates compared to anti-TNF but without significant difference.
ConclusionThe 1-year maintenance findings suggested, in line with our previous induction phase data, only moderate long-term effectiveness in both groups. However, besides the significant response data, VDZ showed numerically higher remission rates compared to anti-TNF though only borderline significant. The higher treatment persistence of VDZ vs anti-TNF, along with the higher effectiveness, may suggest VDZ as a first-line biologic therapy option in UC patients.


Making a Case for Case Reports: The ECCO-CONFER Viewpoint on Investigating Rare Events in a Medical World Reigned by Group-comparative StatisticsYear: 2017
Source: JCC: Volume 11, Issue 2, 2017
Authors: Konstantinos H. Katsanos, Eugeni Domènech, Jean-François Rahier, Uri Kopylov, Gionata Fiorino, Gerhard Rogler, Edouard Louis, Shomron Ben-Horin
Created: Friday, 22 February 2019, 10:55 AM by ECCO Administrator
Progress in medicine has been made in the past primarily through the clinical experience of physicians and uncontrolled observations. With the advent of medical journals, knowledge dissemination and much of medical progress had been made possible through clinical reports and meticulous observations on cases or series of cases. This was true for many medical breakthroughs, including the initial paper by Burrill Crohn, Leon Ginzburg and Gordon Oppenheimer, who described their observations of a mere 14 surgical patients with ‘regional ileitis’, which later became known as Crohn’s disease.1 However in recent decades, the controlled clinical trial gained primacy as the holy grail of evidence-based medicine, and observational studies similarly became subject to stricter and preferably comparative statistical methodology in the forms of population-based studies, prospective cohorts or retrospective case-control studies. This trend, towards comparative and preferably controlled research methodology as the prevailing dogma, has led to case reports falling out of favour with the medical scientific community touting its potential caveats of chance associations and susceptibility to many uncontrolled confounders. Coupled with the fact that case reports may create less citation potential, which is necessary for a journal impact factor and citation index standing, case reports and case series have also found it increasingly difficult to be published.2 Indeed most leading gastroenterology journals, JCC included, now generally refrain from publishing case reports or small case series.
Management of Paediatric Ulcerative Colitis, Part 1: Ambulatory Care—An Evidence-based Guideline From European Crohn's and Colitis Organization and European Society of Paediatric Gastroenterology, Hepatology and NutritionYear: 2018
Source: JPGN: Volume 67, Issue 2, 2018
Authors: Turner, Dan; Ruemmele, Frank M.; Orlanski-Meyer, Esther; Griffiths, Anne M.; de Carpi, Javier Martin; Bronsky, Jiri; Veres, Gabor; Aloi, Marina; Strisciuglio, Caterina; Braegger, Christian P.; Assa, Amit; Romano, Claudio; Hussey, Séamus; Stanton, Michael; Pakarinen, Mikko; de Ridder, Lissy; Katsanos, Konstantinos; Croft, Nick; Navas-López, Victor; Wilson, David C.; Lawrence, Sally; Russell, Richard K.
Created: Friday, 31 August 2018, 11:02 AM by Dauren Ramankulov
These guidelines provide a guide to clinicians managing children with UC and IBD-unclassified management to provide modern management strategies while maintaining vigilance around appropriate outcomes and safety issues.
Management of Paediatric Ulcerative Colitis, Part 2: Acute Severe Colitis—An Evidence-based Consensus Guideline From the European Crohn's and Colitis Organization and the European Society of Paediatric Gastroenterology, Hepatology and NutritionYear: 2018
Source: JPGN: Volume 67, Issue 2, 2018
Authors: Turner, Dan; Ruemmele, Frank M.; Orlanski-Meyer, Esther; Griffiths, Anne M.; de Carpi, Javier Martin; Bronsky, Jiri; Veres, Gabor; Aloi, Marina; Strisciuglio, Caterina; Braegger, Christian P.; Assa, Amit; Romano, Claudio; Hussey, Séamus; Stanton, Michael; Pakarinen, Mikko; de Ridder, Lissy; Katsanos, Konstantinos H.; Croft, Nick; Navas-López, Víctor Manuel; Wilson, David C.; Lawrence, Sally; Russell, Richard K.
Created: Friday, 31 August 2018, 11:19 AM by Dauren Ramankulov
Last Modified: Thursday, 21 February 2019, 6:02 PM by ECCO Administrator
Background and aim: Acute severe colitis (ASC) is one of the few emergencies in pediatric gastroenterology. Tight monitoring and timely medical and surgical interventions may improve outcomes and minimize morbidity and mortality. We aimed to standardize daily treatment of ASC in children through detailed recommendations and practice points which are based on a systematic review of the literature and consensus of experts.
Management of Patients on ThiopurinesYear: 2015
Source: Talking Heads
Authors: Antonio Lopéz San-Román, Eugeni Domènech
Created: Friday, 22 February 2019, 4:35 PM by ECCO Administrator
Last Modified: Friday, 13 January 2023, 11:31 AM by ECCO Administrator
Management of Pediatric Ulcerative Colitis: Joint ECCO and ESPGHAN Evidence-based Consensus GuidelinesYear: 2012
Source: JPGN: Volume 55, Issue 3, 2012
Authors: Turner, Dan; Levine, Arie; Escher, Johanna C.; Griffiths, Anne M.; Russell, Richard K.; Dignass, Axel; Dias, Jorge Amil; Bronsky, Jiri; Braegger, Christian P.; Cucchiara, Salvatore; de Ridder, Lissy; Fagerberg, Ulrika L.; Hussey, Séamus; Hugot, Jean-Pierre; Kolacek, Sanja; Kolho, Kaija Leena; Lionetti, Paolo; Pærregaard, Anders; Potapov, Alexander; Rintala, Risto; Serban, Daniela E.; Staiano, Annamaria; Sweeny, Brian; Veerman, Gigi; Veres, Gabor; Wilson, David C. Ruemmele, Frank M.
Created: Thursday, 30 August 2018, 11:25 AM by Dauren Ramankulov
The aim of this new consensus is to establish standards for the diagnosis and management of Paediatric UC. It will include the use of immunosuppressors and biologics.
Management of perianal CDYear: 2019
Source: 17th IBD Intensive Advanced Course
Authors: Antonio López-Sanromán, Paulo Kotze
Created: Tuesday, 28 May 2019, 3:32 PM
Files: 1
Management of refractory pouchitisYear: 2017
Source: 15th IBD Intensive Advanced Course
Authors: Dotan I.
Last Modified: Tuesday, 18 May 2021, 9:54 AM by ECCO Administrator
Files: 1
Management of stomaYear: 2018
Source: 3rd D-ECCO Workshop
Authors: Wierdsma Nicolette
Created: Tuesday, 8 May 2018, 11:36 AM
Files: 1