Exabis Library
Welcome to the e-CCO Library!
Nursing Perspectives: Stoma & Pouch: Part I
2016
Talking Heads
Friday, 22 February 2019, 4:11 PM by ECCO Administrator
Friday, 13 January 2023, 11:58 AM by ECCO Administrator
'Mainstream' biologicals: When to use?
2022
6th Basic ECCO: EduCational COurse for Industry
Tuesday, 24 May 2022, 8:13 PM
'New' kids on the block
2022
6th Basic ECCO: EduCational COurse for Industry
Tuesday, 24 May 2022, 8:13 PM
'Older' medication: Still useful?
2022
6th Basic ECCO: EduCational COurse for Industry
Tuesday, 24 May 2022, 8:13 PM
'Special' treatments
2022
6th Basic ECCO: EduCational COurse for Industry
Tuesday, 24 May 2022, 8:13 PM
10 years of surgery for Crohn's perineal disease
2021
10th S-ECCO IBD Masterclass
Friday, 1 October 2021, 12:41 PM
10 years of surgery for intestinal Crohn's Disease
2021
10th S-ECCO IBD Masterclass
Friday, 1 October 2021, 12:41 PM
10 years of surgery for Ulcerative Colitis
2021
10th S-ECCO IBD Masterclass
Friday, 1 October 2021, 12:41 PM
2nd Edition of Top Strategy Trials
2019
Talking Heads
Friday, 6 September 2019, 3:24 PM by Dauren Ramankulov
Wednesday, 2 June 2021, 12:00 PM by ECCO Administrator
3rd Edition of Top Strategy Trials
2020
Talking Heads
Monday, 27 July 2020, 11:54 AM by Dauren Ramankulov
Wednesday, 2 June 2021, 12:25 PM by ECCO Administrator
3rd line rescue in Acute severe UC - safe and effective?
2019
JCC Podcast
Monday, 2 September 2019, 4:22 PM by Dauren Ramankulov
Wednesday, 4 March 2020, 12:13 PM by Dauren Ramankulov
5-ASA compounds
2017
15th IBD Intensive Advanced Course
Friday, 16 April 2021, 2:43 PM by ECCO Administrator
1
A comparative efficacy and safety analysis of subcutaneous infliximab and vedolizumab in patients with Crohn’s Disease and Ulcerative Colitis
2022
ECCO'22 Virtual
Tuesday, 24 May 2022, 8:13 PM
A multi-centre study to explore the prevalence of Inflammatory Bowel Disease indicators in patients with moderate- to- severe psoriasis: Baseline results from the EPIC study
2022
ECCO'22 Virtual
Tuesday, 24 May 2022, 8:13 PM
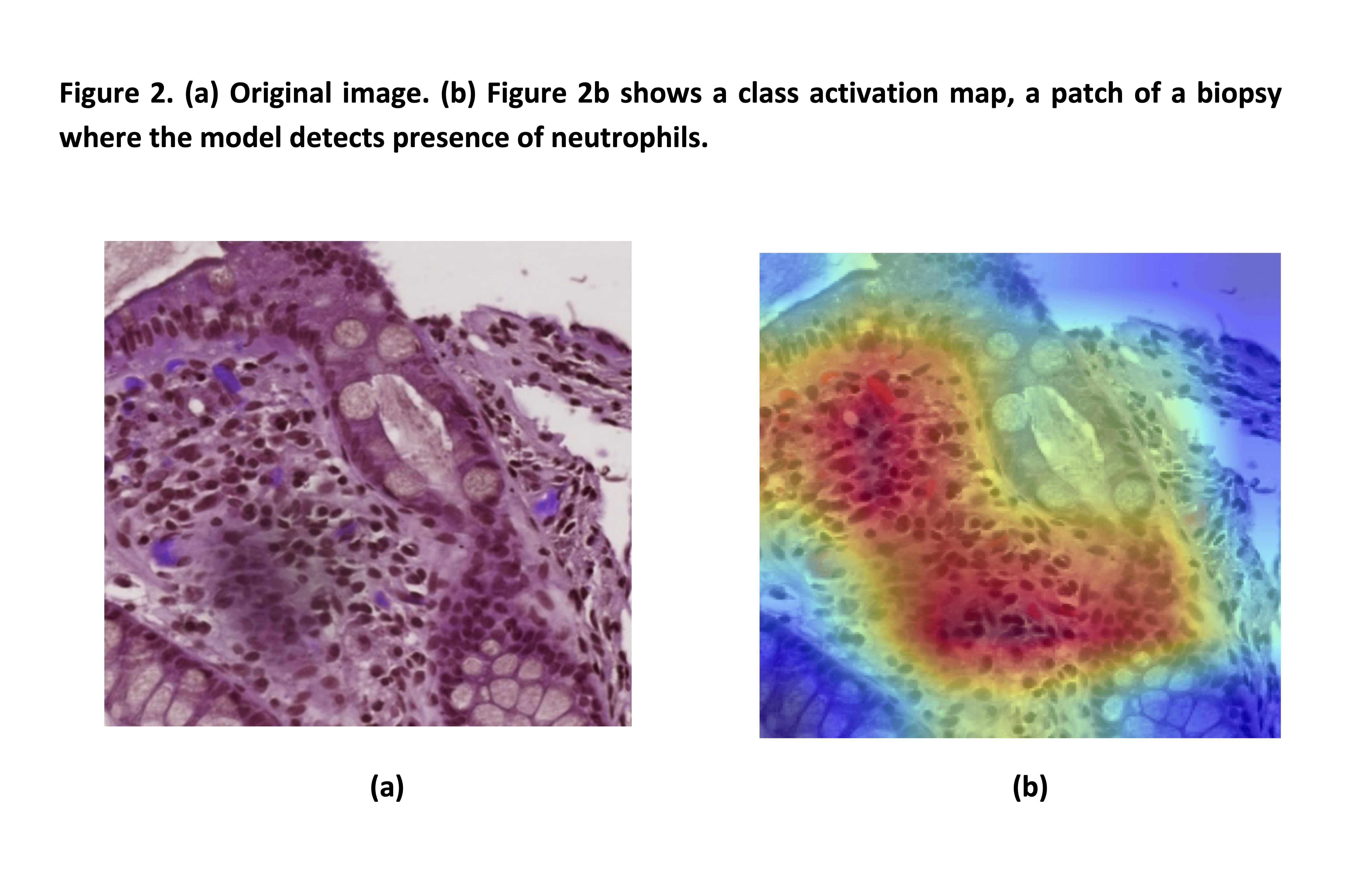
A new simplified histology artificial intelligence system for accurate assessment of remission in Ulcerative Colitis
2022
ECCO'22 Virtual
Tuesday, 24 May 2022, 8:13 PM
A novel predictive scoring system of venous thromboembolism after surgery for Inflammatory Bowel Disease: A NSQIP-IBD registry analysis
2022
ECCO'22 Virtual
Tuesday, 24 May 2022, 8:13 PM
A Phase 1 Study Evaluating the Bioequivalence of the Proposed Commercial and Clinical Formulations of Etrasimod 2mg, and the Effect of Food on the Pharmacokinetics of the Proposed Commercial Formulation in Healthy Volunteers
2022
ECCO'22 Virtual
Tuesday, 24 May 2022, 8:13 PM






 Conclusion
Conclusion