Exabis Library
Welcome to the e-CCO Library!
OP22: The risk of cancer in pediatric-onset immune-mediated inflammatory diseases – a nationwide Danish study from 1980-2018.
2023
ECCO’23 Copenhagen
Friday, 14 July 2023, 2:22 PM
OP22: The risk of cancer in pediatric-onset immune-mediated inflammatory diseases – a nationwide Danish study from 1980-2018.
2023
ECCO’23 Copenhagen
Friday, 14 July 2023, 10:43 AM
OP22: Topical Sphingosine-1-Phosphate (S1P) Receptor 1 Modulation Regulates Gut Angiogenesis in Inflammatory Bowel Diseases
2024
ECCO'24 Stockholm
Tuesday, 30 April 2024, 5:03 PM
OP23 Efficacy and safety of vedolizumab SC in patients with moderately to severely active Crohn’s disease: Results of the VISIBLE 2 study
2020
ECCO'20 Vienna
Thursday, 30 January 2020, 10:12 AM
OP23: Asymptomatic inflammatory bowel disease diagnosed during the colorectal cancer population screening in Catalonia
2023
ECCO’23 Copenhagen
Friday, 14 July 2023, 2:22 PM
OP23: Asymptomatic inflammatory bowel disease diagnosed during the colorectal cancer population screening in Catalonia
2023
ECCO’23 Copenhagen
Friday, 14 July 2023, 10:43 AM
OP23: CKD-506, a novel histone deacetylase (HDAC) 6 inhibitor, ameliorates colitis in various animal models
2019
ECCO'19 Copenhagen
Tuesday, 28 May 2019, 3:32 PM
1
OP23: CKD-506, a novel histone deacetylase (HDAC) 6 inhibitor, ameliorates colitis in various animal models
2019
ECCO '19 Copenhagen
Friday, 22 February 2019, 9:41 AM
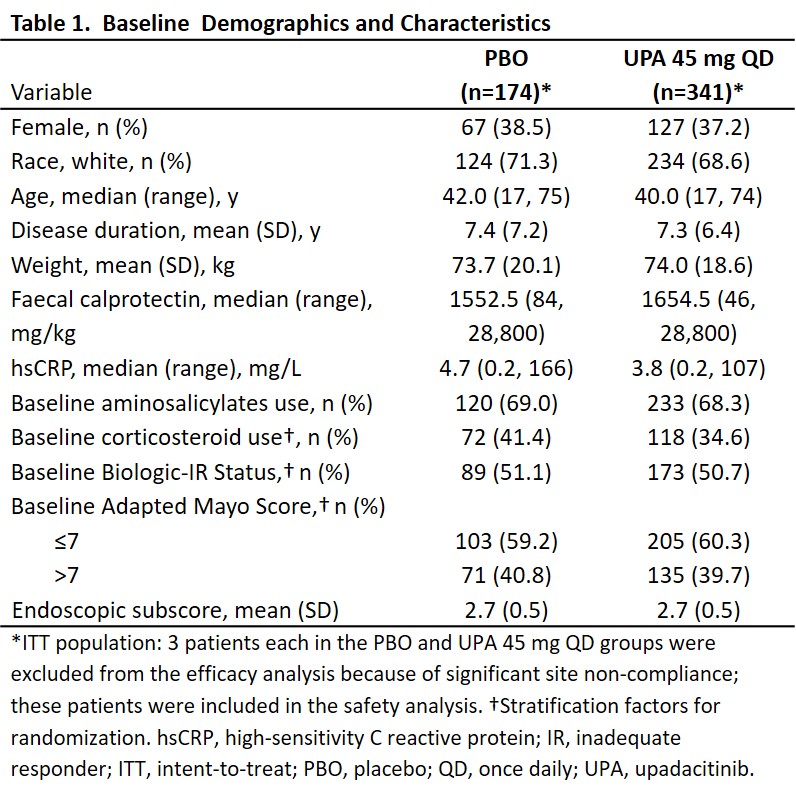
OP23: Efficacy and safety of upadacitinib as induction therapy in patients with Moderately to Severely Active Ulcerative Colitis: Results from phase 3 U-ACCOMPLISH study
2021
ECCO'21 Virtual
Wednesday, 2 June 2021, 4:12 PM
OP23: Efficacy and safety of upadacitinib as induction therapy in patients with Moderately to Severely Active Ulcerative Colitis: Results from phase 3 U-ACCOMPLISH study
2021
ECCO'21 Virtual
Friday, 1 October 2021, 12:41 PM
OP23: Efficacy and safety of vedolizumab SC in patients with Moderately to Severely active Crohn’s Disease: Results of the VISIBLE 2 study
2020
ECCO'20 Vienna
Tuesday, 23 June 2020, 5:40 PM
OP23: Efficacy and safety of vedolizumab SC in patients with Moderately to Severely active Crohn’s Disease: Results of the VISIBLE 2 study
2020
ECCO'20 Vienna
Tuesday, 23 June 2020, 4:58 PM
1
OP23: Guselkumab induction restores intestinal immune homeostasis and promotes epithelial repair in moderately to severely active Ulcerative Colitis
2024
ECCO'24 Stockholm
Tuesday, 30 April 2024, 5:03 PM
OP23: The efficacy and safety of guselkumab induction therapy in patients with moderately to severely active Ulcerative Colitis: Phase 2b QUASAR Study results through week 12
2022
ECCO'22
Friday, 11 February 2022, 3:52 PM
OP24 A novel subcutaneous infliximab (CT-P13): 1-year results including switching results from intravenous infliximab (CT-P13) in patients with active Crohn’s disease and ulcerative colitis
2020
ECCO'20 Vienna
Thursday, 30 January 2020, 10:12 AM
OP24: A novel subcutaneous infliximab (CT-P13): 1-year results including switching results from intravenous infliximab (CT-P13) in patients with active Crohn’s Disease and Ulcerative Colitis
2020
ECCO'20 Vienna
Tuesday, 23 June 2020, 5:40 PM
OP24: A novel subcutaneous infliximab (CT-P13): 1-year results including switching results from intravenous infliximab (CT-P13) in patients with active Crohn’s Disease and Ulcerative Colitis
2020
ECCO'20 Vienna
Tuesday, 23 June 2020, 4:58 PM
1
OP24: Clinical efficacy and safety of guselkumab maintenance therapy in patients with moderately to severely active Crohn’s Disease: Week 48 analyses from the phase 2 GALAXI 1 study
2022
ECCO'22
Friday, 11 February 2022, 3:52 PM
OP24: Effectiveness and safety of ustekinumab 90 mg every 4 weeks in Crohn’s disease
2019
ECCO '19 Copenhagen
Friday, 22 February 2019, 9:41 AM
OP24: Effectiveness and safety of ustekinumab 90 mg every four weeks in Crohn's disease
2019
ECCO'19 Copenhagen
Tuesday, 28 May 2019, 3:32 PM
1