Exabis Library
Welcome to the e-CCO Library!
Clinical features of IBD-related tumours
2019
4th H-ECCO IBD Masterclass
Tuesday, 28 May 2019, 3:32 PM
1
Clinical outcomes of COVID-19 and Impact on Disease Course in Patients with Inflammatory Bowel Disease
2022
ECCO'22 Virtual
Tuesday, 24 May 2022, 8:13 PM
Clinical trial coordinator's view
2019
3rd School for Clinical Trialists
Tuesday, 28 May 2019, 3:32 PM
1
Clinical trials: Lessons from the past
2021
5th Advanced ECCO: EduCational COurse for Industry
Friday, 1 October 2021, 12:41 PM
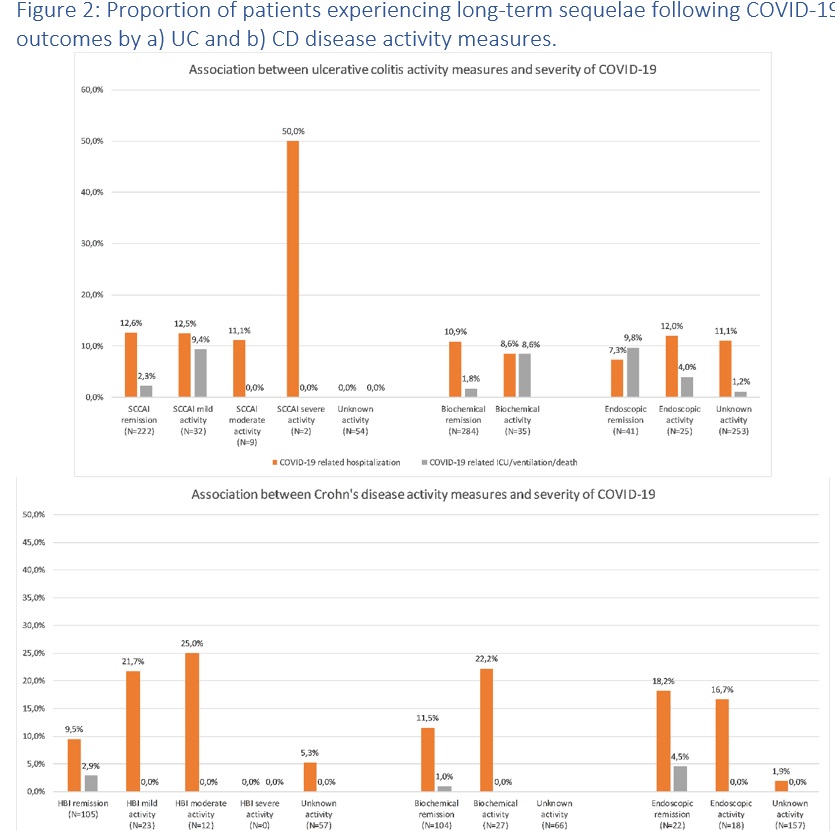
Clinical, biochemical and endoscopic disease activity of Inflammatory Bowel Diseases are not associated with the severity or long-term outcomes of COVID-19 – A Danish prospective population-based cohort study
2022
ECCO'22 Virtual
Tuesday, 24 May 2022, 8:13 PM
Closing remarks, N-ECCO in 2018 and beyond
2018
12th N-ECCO Network Meeting
Friday, 23 March 2018, 12:23 PM
1
CMV: Identification and quantification
2018
3rd H-ECCO IBD Masterclass
Tuesday, 8 May 2018, 11:36 AM
1
Colonic versus small bowel CD: Same mechanism - same treatment?
2020
ECCO'20 Vienna
Tuesday, 23 June 2020, 5:40 PM
Colonic versus small bowel CD: Same mechanism - same treatment?
2020
ECCO'20 Vienna
Tuesday, 23 June 2020, 4:58 PM
1
Colorectal cancer in inflammatory bowel disease: Results of the 3rd ECCO pathogenesis scientific workshop (I)
2014
JCC: Volume 8, Issue 1, 2014
Friday, 22 February 2019, 1:41 PM by ECCO Administrator
Combinations of biologics, and small molecules and biologics
2020
7th ClinCom Workshop
Tuesday, 23 June 2020, 4:58 PM
1
Combined approach for intestinal sparing in CD?
2017
ECCO'17 Barcelona
Wednesday, 15 March 2017, 2:50 PM by ECCO Administrator
1

 Conclusion
Conclusion

 Conclusion
Conclusion