Exabis Library
Welcome to the e-CCO Library!
The child with IBD: Should anti-TNF be used as a mono-therapy in children (safety risk)? Who should (be allowed to) operate on the children in IBD?
2017
ECCO'17 Barcelona
Friday, 17 March 2017, 9:51 AM by Vesna Babaja
1
The contribution of ultrasound in Ulcerative Colitis
2019
6th ECCO-ESGAR Ultrasound Workshop - Advanced
Wednesday, 5 June 2019, 9:01 PM
The contribution of ultrasound in Ulcerative Colitis
2019
6th ECCO-ESGAR Ultrasound Workshop - Advanced
Tuesday, 28 May 2019, 3:32 PM
1
The COSTA study: COlonic Salvage by Therapeutic Appendectomy
2021
10th S-ECCO IBD Masterclass
Friday, 1 October 2021, 12:41 PM
The crazy stuff - what your patients are taking and why?
2019
ECCO'19 Copenhagen
Tuesday, 28 May 2019, 3:32 PM
1
The effects of maintenance therapy with upadacitinib on abdominal pain, bowel urgency, and fatigue in patients with moderately to severely active Ulcerative Colitis: Phase 3 U-ACHIEVE maintenance results
2022
ECCO'22 Virtual
Tuesday, 24 May 2022, 8:13 PM
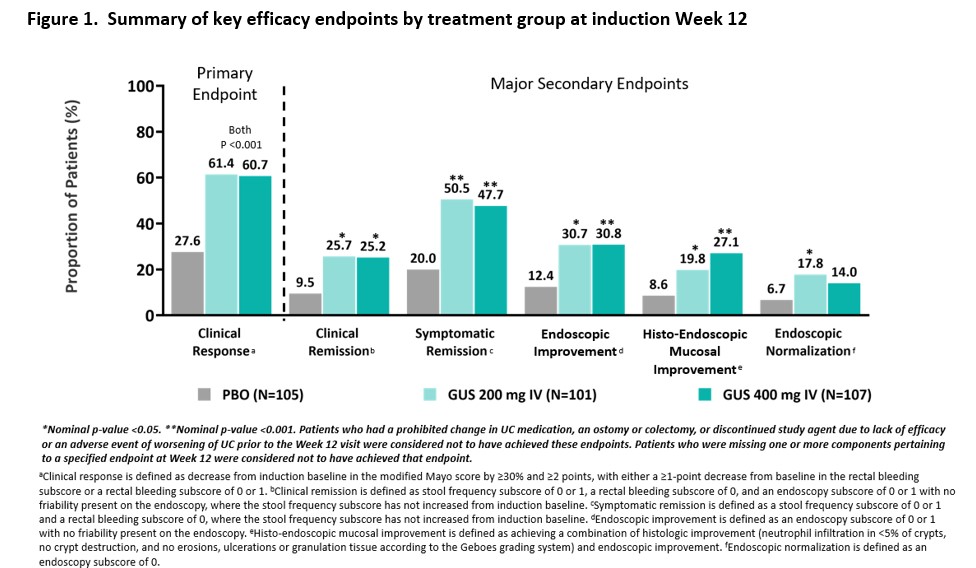
The efficacy and safety of guselkumab induction therapy in patients with moderately to severely active Ulcerative Colitis: Phase 2b QUASAR Study results through week 12
2022
ECCO'22 Virtual
Tuesday, 24 May 2022, 8:13 PM
The elderly patient with IBD: Should azathioprine ever be used in the elderly? Should the type of surgery be different in an elderly patient?
2017
ECCO'17 Barcelona
Wednesday, 15 March 2017, 2:02 PM by ECCO Administrator
1
The extracellular matrix as a central regulator of intestinal regeneration
2019
7th SciCom Workshop: Mechanisms and therapeutic modulation of mucosal healing in IBD
Tuesday, 28 May 2019, 3:32 PM
1
The First European Evidence-based Consensus on Extra-intestinal Manifestations in Inflammatory Bowel Disease
2016
JCC: Volume 10, Issue 3, 2016
Friday, 31 August 2018, 10:10 AM by Dauren Ramankulov
The first virtual chromoendoscopy artificial intelligence system to detect endoscopic and histologic remission in Ulcerative Colitis
2022
ECCO'22 Virtual
Tuesday, 24 May 2022, 8:13 PM
The forgotten populations in the gut
2017
ECCO'17 Barcelona
Wednesday, 15 March 2017, 2:00 PM by ECCO Administrator
1
The future of using nutrition to alter the microbiome
2021
6th D-ECCO Workshop
Friday, 1 October 2021, 12:41 PM
The IBD-BOOST programme: Developing a digital self-management intervention for symptoms of fatigue, pain and urgency in Inflammatory Bowel Disease
2020
14th N-ECCO Network Meeting
Tuesday, 23 June 2020, 4:58 PM
1
The ileorectal anastomosis in UC: Time for a comeback?
2017
ECCO'17 Barcelona
Wednesday, 15 March 2017, 2:46 PM by ECCO Administrator
1
The implementation of prognostic factors to manage and modify outcomes - case based discussion
2022
6th EpiCom Workshop
Tuesday, 24 May 2022, 8:13 PM
The importance of shared care in IBD - a tandem talk
2019
13th N-ECCO Network Meeting
Tuesday, 28 May 2019, 3:32 PM
1
The importance of the multidisciplinary team (MDT) and its impact on quality of life and medication adherence in patients with Inflammatory Bowel Disease
2022
16th N-ECCO Network Meeting
Tuesday, 24 May 2022, 8:13 PM




 Conclusion
Conclusion


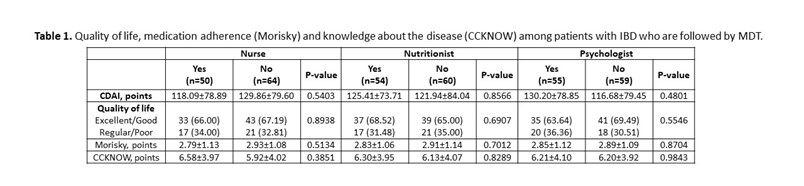 In total, 69 (60.53%) patients with CD and 45 (39.47%) patients with UC were included. The mean age was 39.16 (±13.50) years and 58.77% were female. The disease duration was 9.88 (±7.35) years. Presence of comorbidities was observed in 52.63% patients. About 57 (82.61%) patients with CD use biological therapy, with a statistical difference (p <0.0001) when compared to patients with UC (37.78%). The gastroenterologist was considered very important by 91.23% of patients, coloproctologist by 62.07% of patients, nurse by 65.05% of patients, nutritionist by 50% of patients and psychologist by 47.25% of patients. In the analysis of QoL, 24 (21.05%) patients had excellent QoL, 52 (45.61%) had good QoL, 29 (25.44%) had regular QoL and 9 (7.89%) had poor QoL, with no difference between patients who followed with nurses or other MDT professionals (Table 1). Medication adherence was low in 58.88% of patients. Knowledge about the disease was low (6.21 ± 3.99 points), being higher among patients with CD (p = 0.01). Patients identify the doctor as the main provider of care for their health, but about 10% leave with doubts from their appointments. 10% of patients think that more care with the nurse is necessary and less than 10% of patients are clarified by the nurse about QoL, ostomies, fecal incontinence, disease activity, biological therapy and sexuality.
In total, 69 (60.53%) patients with CD and 45 (39.47%) patients with UC were included. The mean age was 39.16 (±13.50) years and 58.77% were female. The disease duration was 9.88 (±7.35) years. Presence of comorbidities was observed in 52.63% patients. About 57 (82.61%) patients with CD use biological therapy, with a statistical difference (p <0.0001) when compared to patients with UC (37.78%). The gastroenterologist was considered very important by 91.23% of patients, coloproctologist by 62.07% of patients, nurse by 65.05% of patients, nutritionist by 50% of patients and psychologist by 47.25% of patients. In the analysis of QoL, 24 (21.05%) patients had excellent QoL, 52 (45.61%) had good QoL, 29 (25.44%) had regular QoL and 9 (7.89%) had poor QoL, with no difference between patients who followed with nurses or other MDT professionals (Table 1). Medication adherence was low in 58.88% of patients. Knowledge about the disease was low (6.21 ± 3.99 points), being higher among patients with CD (p = 0.01). Patients identify the doctor as the main provider of care for their health, but about 10% leave with doubts from their appointments. 10% of patients think that more care with the nurse is necessary and less than 10% of patients are clarified by the nurse about QoL, ostomies, fecal incontinence, disease activity, biological therapy and sexuality.