Exabis Library
Welcome to the e-CCO Library!
Proteases, PAR2 and Pouchitis
2019
JCC Podcast
Monday, 2 September 2019, 3:58 PM by Dauren Ramankulov
Friday, 28 February 2020, 1:34 PM by Dauren Ramankulov
Psychological Issues in IBD
2019
Educational Audio Podcasts
Friday, 28 February 2020, 3:56 PM by Dauren Ramankulov
Friday, 13 January 2023, 12:26 PM by ECCO Administrator
Psychosocial implications of living with IBD
2017
8th N-ECCO School
Wednesday, 15 March 2017, 1:43 PM by Vesna Babaja
1
Psychosocial implications of living with IBD
2020
11th N-ECCO School
Tuesday, 23 June 2020, 5:40 PM
Wednesday, 16 June 2021, 4:42 PM by ECCO Administrator
Psychosocial implications of living with IBD
2021
12th N-ECCO School
Friday, 1 October 2021, 12:41 PM
Pulmonary manifestations of IBD & its differential diagnosis
2022
7th H-ECCO IBD Masterclass
Tuesday, 24 May 2022, 8:13 PM
Putting GRADE into practice - some examples of workflow
2021
2nd Guideline Methodology and GRADE Workshop
Friday, 1 October 2021, 12:41 PM
Pyroptosis Inhibition Prevents the Cytotoxicity Induced by IL-17 Without Impairing Its Beneficial Effects
2022
ECCO'22 Virtual
Tuesday, 24 May 2022, 8:13 PM
Rapidity of ozanimod-induced symptomatic response and remission in patients with moderately to severely active Ulcerative Colitis: Results from the induction period of True North
2022
ECCO'22 Virtual
Tuesday, 24 May 2022, 8:13 PM
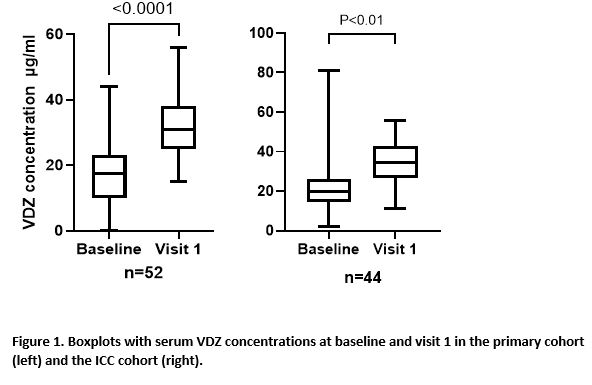
Real World Effectiveness, Safety and Pharmacokinetics of Switching Intravenous Vedolizumab Maintenance treatment to Subcutaneous Vedolizumab Therapy for Inflammatory Bowel Disease
2022
ECCO'22 Virtual
Tuesday, 24 May 2022, 8:13 PM
Real-world multicenter comparison of effectiveness between tofacitinib and vedolizumab in patients with Ulcerative Colitis after failure to at least one anti-TNF agent
2022
ECCO'22 Virtual
Tuesday, 24 May 2022, 8:13 PM
Recreating the intestine ex vivo - Where are we on the way to the artificial gut (organoids, etc.)
2017
5th SciCom Workshop: Methodology on Research
Wednesday, 15 March 2017, 1:37 PM by ECCO Administrator
1